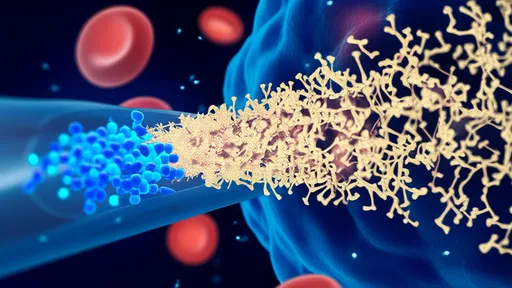
In the rapidly evolving landscape of cancer immunotherapy, CAR-T cell therapy has emerged as a groundbreaking approach, offering new hope to patients with refractory or relapsed malignancies. This innovative treatment involves engineering a patient's own T cells to express chimeric antigen receptors (CARs) that specifically target tumor-associated antigens, thereby harnessing the power of the immune system to combat cancer. While the initial successes of CAR-T therapy, particularly in hematologic cancers like acute lymphoblastic leukemia and certain lymphomas, have been nothing short of revolutionary, challenges remain in enhancing its efficacy, safety, and applicability across a broader range of cancers. As researchers delve deeper into the mechanisms and limitations of current CAR-T protocols, a multitude of optimization strategies are being explored to overcome these hurdles and unlock the full potential of this transformative treatment.
One of the primary areas of focus in optimizing CAR-T therapy is improving the design of the chimeric antigen receptors themselves. Early-generation CARs were relatively simple in structure, but they often led to limited persistence of the engineered cells and suboptimal anti-tumor activity. To address this, scientists are developing next-generation CARs with more sophisticated architectures. For instance, incorporating costimulatory domains such as CD28 or 4-1BB has been shown to enhance T cell proliferation, persistence, and cytokine production. Furthermore, the exploration of multi-specific CARs—those capable of recognizing more than one antigen—is gaining traction. This approach can help mitigate antigen escape, a common phenomenon where tumors downregulate or lose the target antigen, leading to treatment resistance. By targeting multiple antigens simultaneously, these advanced CARs offer a more robust and durable response, reducing the likelihood of relapse.
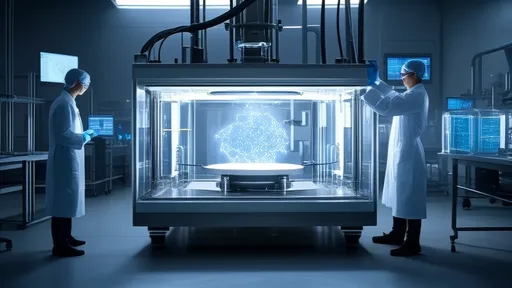
Another critical aspect of optimization lies in enhancing the manufacturing process of CAR-T cells. The current autologous approach, where T cells are harvested from the patient, genetically modified, expanded ex vivo, and then reinfused, is not only time-consuming but also fraught with variability. This can result in inconsistent product quality and potency, ultimately affecting clinical outcomes. To streamline production, researchers are investigating allogeneic, or "off-the-shelf," CAR-T cells derived from healthy donors. These universal CAR-T products could be manufactured in large batches, ensuring consistency and availability, while also reducing the time between diagnosis and treatment. However, this approach comes with its own set of challenges, particularly the risk of graft-versus-host disease and host immune rejection. Advances in gene editing technologies, such as CRISPR-Cas9, are being employed to knock out genes responsible for these adverse effects, paving the way for safer and more effective allogeneic therapies.
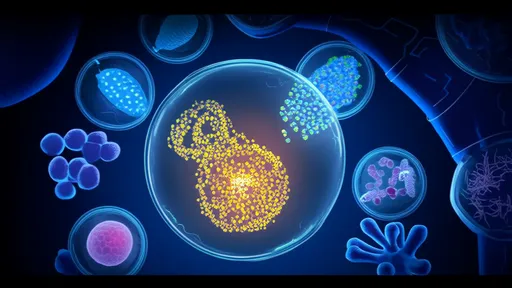
The tumor microenvironment (TME) represents a significant barrier to the success of CAR-T therapy, especially in solid tumors. The immunosuppressive nature of the TME can inhibit the function and persistence of CAR-T cells, leading to treatment failure. Strategies to overcome this include engineering CAR-T cells to resist immunosuppressive factors such as TGF-β or PD-L1. For example, CARs equipped with dominant-negative receptors for TGF-β or checkpoint inhibitors can help the engineered cells maintain their cytotoxic activity even in hostile environments. Additionally, combining CAR-T therapy with other modalities, such as immune checkpoint blockers or targeted agents, is showing promise in clinical trials. These combinations can reprogram the TME to be more permissive to T cell activity, thereby enhancing the overall anti-tumor response.
Safety remains a paramount concern in CAR-T therapy, particularly with the risk of severe toxicities like cytokine release syndrome (CRS) and neurotoxicity. These adverse events are often driven by the rapid activation and proliferation of CAR-T cells, leading to an overwhelming inflammatory response. To mitigate these risks, researchers are developing safety switches—suicide genes or mechanisms that allow for the controlled elimination of CAR-T cells in case of severe toxicity. One such approach involves incorporating inducible caspase-9 (iCasp9) systems, which can be activated by a small molecule to trigger apoptosis in the engineered cells. Another strategy is the use of bispecific CARs that require dual antigen recognition for full activation, thereby increasing specificity and reducing off-target effects. These safety enhancements are crucial for expanding the use of CAR-T therapy to a wider patient population, including those with comorbidities who may be more vulnerable to severe side effects.
Beyond engineering the CAR-T cells themselves, optimizing the conditioning regimens administered to patients prior to infusion is also vital. Lymphodepleting chemotherapy, commonly used to create space and reduce regulatory T cells, can significantly impact the expansion and persistence of CAR-T cells. However, the intensity and timing of these regimens need fine-tuning to maximize benefits while minimizing toxicity. Studies are exploring alternative conditioning agents or combinations that could better prepare the immune environment for CAR-T cell engraftment and function. Personalized approaches, tailored to the patient's immune status and disease characteristics, may further improve outcomes by ensuring that the host environment is optimally primed for therapy.
Looking ahead, the integration of artificial intelligence and machine learning into CAR-T therapy development holds immense promise. These technologies can analyze vast datasets from clinical trials and preclinical studies to identify patterns and predictors of response, toxicity, and resistance. By leveraging such insights, researchers can design more effective CAR constructs, identify ideal target antigens, and develop personalized treatment protocols. Moreover, AI-driven platforms can optimize manufacturing processes by predicting the best conditions for T cell expansion and transduction, leading to higher-quality products. As these tools become more sophisticated, they will undoubtedly play a pivotal role in accelerating the translation of CAR-T therapy from bench to bedside.
In conclusion, the optimization of CAR-T cell therapy is a multifaceted endeavor that requires innovations across various domains—from CAR design and manufacturing to overcoming the immunosuppressive tumor microenvironment and enhancing safety measures. While significant progress has been made, ongoing research and clinical trials continue to push the boundaries of what is possible. The collaborative efforts of scientists, clinicians, and industry partners are essential to addressing the remaining challenges and realizing the full potential of CAR-T therapy. As these optimization strategies mature, they promise to not only improve outcomes for patients with hematologic malignancies but also expand the reach of CAR-T therapy to solid tumors, ultimately transforming the standard of care in oncology and offering new avenues for hope and healing.

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025
By /Aug 25, 2025
By /Aug 25, 2025
By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025
By /Aug 25, 2025
By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025
By /Aug 25, 2025

By /Aug 25, 2025
By /Aug 25, 2025
By /Aug 25, 2025

By /Aug 25, 2025

By /Aug 25, 2025
By /Aug 25, 2025